Neuromusculoskeletal disorders (NMSDs) affect millions of people worldwide, impacting the body’s ability to move, coordinate, and function with ease. These conditions, involving the complex interplay between the nervous system, muscles, and skeletal system, can range from minor discomfort to debilitating pain and long-term disability. Understanding what NMSDs are, what causes them, and how to effectively manage them is essential for maintaining a healthy, active life.
Unlike acute injuries like a sprained ankle or a broken bone, NMSDs often develop gradually due to repetitive strain, poor posture, underlying neurological conditions, or chronic inflammation. Whether it’s the stiffness from arthritis, nerve pain from a herniated disc, or muscle weakness caused by neurological diseases, these disorders can significantly reduce quality of life if left unaddressed.
What Are Neuromusculoskeletal Disorders?
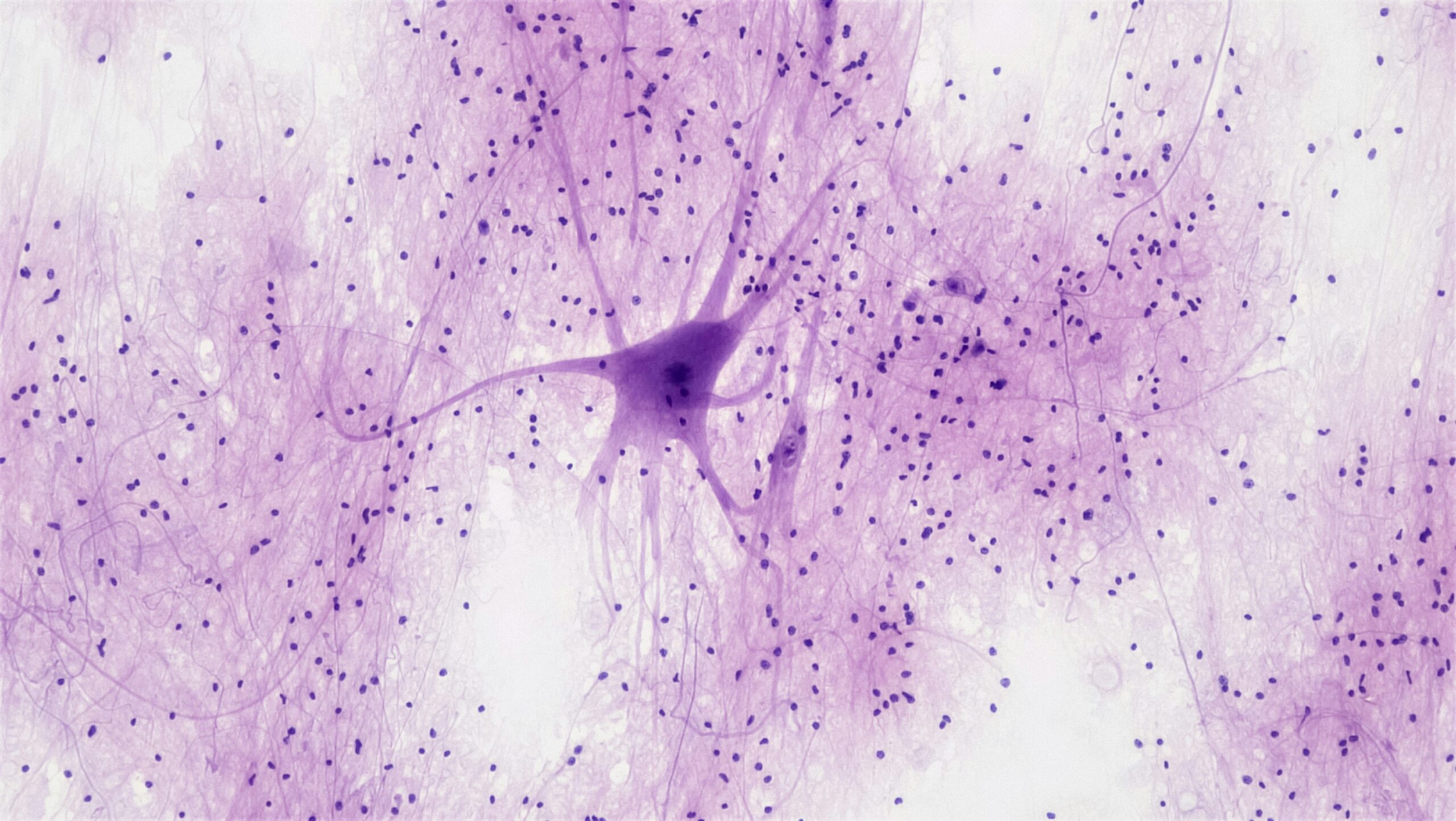
Neuromusculoskeletal disorders are conditions that impact the nerves (neuro), muscles (musculoskeletal), and bones/joints (skeletal) of the body. They are characterized by pain, functional limitations, and restricted mobility. These disorders are diverse and may involve one or more components of the system.
Some common NMSDs include:
Low back pain
Sciatica
Cervical spondylosis
Carpal tunnel syndrome
Osteoarthritis
Rheumatoid arthritis
Fibromyalgia
Parkinson’s disease (with musculoskeletal manifestations)
Muscular dystrophy
Tendinitis and bursitis
Wear and tear, autoimmune reactions, genetic predispositions, trauma, or neurological dysfunction can cause these conditions. Many people experience overlapping symptoms such as numbness, tingling, stiffness, or muscle spasms, making an accurate diagnosis a critical first step in managing the condition.
Recognizing the Symptoms
Early recognition of symptoms is key to preventing long-term complications. People experiencing NMSDs often report persistent pain, weakness, reduced range of motion, or functional difficulties in daily tasks. In some cases, pain may radiate from the spine to the limbs, or patients may feel shooting, burning, or electric-like sensations caused by nerve involvement.
Other signs include muscle cramps, tremors, joint swelling, fatigue, and balance issues. These symptoms may worsen with activity or remain constant, depending on the nature and cause of the disorder.
Suppose symptoms persist for more than a few weeks, interfere with normal function, or are accompanied by neurological signs such as bowel/bladder issues or severe weakness. In that case, it’s crucial to seek medical attention.
Diagnosis and Assessment
Effective management of neuromusculoskeletal disorders begins with a comprehensive diagnosis. Health care providers use a combination of physical examination, medical history, imaging studies, and electrodiagnostic testing to pinpoint the underlying issue.
X-rays, MRI scans, and CT scans provide visual evidence of structural problems such as disc herniations, joint degeneration, or bone deformities. Electromyography (EMG) and nerve conduction studies help assess the function of nerves and muscles, especially in cases involving neuropathy or radiculopathy.
A detailed understanding of the condition allows clinicians to tailor a treatment plan that addresses both the root cause and the patient’s specific needs.
Treatment Approaches
Treatment for NMSDs depends on the type and severity of the condition. Most cases are managed with a combination of non-invasive therapies, lifestyle changes, and targeted interventions. In rare or advanced cases, surgical options may be considered.
Physical therapy is often the cornerstone of treatment. Therapists work with patients to strengthen muscles, improve posture, restore mobility, and reduce pain. Tailored exercise regimens, stretching routines, and manual therapy techniques can make a significant difference in recovery and pain prevention.
Pain management may involve medications such as anti-inflammatories, muscle relaxants, or nerve pain modulators. In some cases, interventional procedures like corticosteroid injections, nerve blocks, or dry needling are used to control symptoms and improve function.
Occupational therapy helps patients adapt to limitations in their daily lives by teaching ergonomic strategies, using assistive devices, and modifying routines to reduce strain.
In addition to conventional treatments, some patients benefit from complementary therapies such as acupuncture, chiropractic care, massage therapy, and yoga. These methods enhance circulation, relieve stress, and support overall well-being when used appropriately.
The Role of Lifestyle and Prevention
Lifestyle choices play a pivotal role in both the development and management of neuromusculoskeletal disorders. Prolonged sitting, poor posture, heavy lifting, repetitive movements, and sedentary habits can strain muscles and joints over time. On the other hand, healthy habits can protect and support the body’s musculoskeletal system.
Regular low-impact exercise, such as walking, swimming, or cycling, helps maintain flexibility, muscle tone, and joint function. Core strengthening and balance training are particularly beneficial for spinal health and fall prevention.
Nutrition also matters. A balanced diet rich in calcium, vitamin D, magnesium, and anti-inflammatory foods supports bone density and muscle repair. Avoiding processed foods and excess sugar can help reduce systemic inflammation, which is often a contributor to chronic pain.
Ergonomics is another key factor. Whether at a desk, behind the wheel, or in a warehouse, using proper body mechanics and ergonomic tools can prevent repetitive strain injuries. Simple changes like adjusting chair height, using a lumbar support, or taking regular breaks to stretch can go a long way in avoiding discomfort.
Sleep quality, hydration, and stress management are often overlooked but essential. Chronic stress can exacerbate muscle tension and pain perception, while dehydration affects muscle performance and joint lubrication.
Emotional and Psychological Impacts
Living with a chronic neuromusculoskeletal disorder can be emotionally taxing. The persistent pain and limitations on mobility often lead to frustration, anxiety, depression, and feelings of isolation. It’s not uncommon for patients to experience a reduced sense of self-worth or withdrawal from social activities.
Addressing the psychological aspects of chronic pain is essential for holistic recovery. Cognitive-behavioral therapy (CBT), mindfulness practices, and support groups can help individuals manage stress, cope with pain, and maintain a positive outlook. Mental health care should be integrated into treatment plans whenever possible.
The Importance of Patient Education
Empowering patients with knowledge about their condition is vital. Understanding the cause of symptoms, the purpose of treatments, and the expectations for recovery encourages active participation in the healing process. Education helps patients make informed decisions, adhere to therapy, and avoid behaviors that may worsen their condition.
Clinicians often emphasize self-care strategies such as home exercises, pacing techniques, posture correction, and the use of hot/cold therapy. A collaborative approach, where patients and providers work together as partners, yields the best outcomes.
Looking Ahead: Advances and Hope
Medical research continues to improve our understanding of neuromusculoskeletal disorders. Advances in regenerative medicine, including stem cell therapy and platelet-rich plasma (PRP), offer potential for tissue repair and pain relief. Wearable technology, telehealth, and robotic rehabilitation tools are enhancing access and personalization in care.
As awareness grows, so does the ability to detect and treat these conditions early, minimizing their long-term impact. With comprehensive care, supportive therapy, and proactive lifestyle management, people with NMSDs can lead fulfilling, active lives.
Neuromusculoskeletal disorders are complex and multifaceted, but they are not insurmountable. Through early diagnosis, multidisciplinary treatment, and active self-care, individuals can reduce pain, improve function, and regain control of their lives. Managing these conditions means more than just responding to pain—it’s about restoring balance, movement, and confidence in every step forward.